Concussions are not limited to sports injuries - they can happen anywhere, at any time. According to the Centers for Disease Control and Prevention (CDC), falls are the #1 cause of concussions. Some of the other common non-athletic causes of concussions include workplace accidents, motor vehicle accidents, and assault / domestic abuse.
There are a few distinctions between athletic and non-athletic concussions to be aware of.
Gap in Concussion Knowledge
Athletes have a working knowledge of concussion signs and symptoms as well as the importance of getting immediate treatment. Many athletes may also have firsthand experience with concussions in either themselves or a teammate.
Non-athletes may not have the same baseline level of concussion knowledge. Thus, they may be less likely to recognize concussion signs and symptoms and more susceptible to believe misinformation.
Less Access to Providers
In athletic populations, there is typically an athletic trainer or someone on the sidelines ready to identify potential concussions and refer for further evaluation right away. In non-athletic populations, individuals may not recognize their symptoms as being from a potential concussion and may not seek treatment for weeks or months after the injury.
Lack of Baseline Testing
Athletes are more likely to have taken an ImPACT baseline test than non-athletes. While having a baseline test is preferred, ImPACT provides normative data based on the patients’ demographics that can be used when baseline test data is not available.
Concussion education is especially important for non-athletic populations who may not have the same baseline level of concussion knowledge as athletes.
Explain to patients that concussion is a metabolic injury rather than a structural injury, and therefore no special tests or imaging will definitely show a concussion. Concussion doesn’t cause bleeding, swelling, or bruising in the brain. Rather, concussion is an energy crisis in the brain which includes neuronal depolarization, release of excitatory neurotransmitters, ionic shifts, changes in glucose metabolism, altered cerebral blood flow, and impaired axonal function.
Because the spread of misinformation has created a lot of hysteria around concussion, patients may be feeling uneasy or fearful about their recovery. It’s important to reassure patients that concussion is a treatable injury and to set realistic expectations for the course of symptoms and length of recovery process.
One way to make sure patients are informed about concussions is to refute some of the common myths.
Myth: Concussion occurs only as a result of a direct blow to the head.
Fact: Concussion may be caused by a direct blow to the head, face, neck, or elsewhere on the body as long as the force of impact is transmitted to the head.
Myth: Concussion occurs only upon experiencing a loss of consciousness
Fact: A concussion can occur with or without a loss of consciousness. In fact, more than 90% of individuals diagnosed with a concussion do not lose consciousness.
Myth: Everyone is at the same risk for concussion.
Fact: Various factors such as gender, medical history, and some other pre-existing risk factors put an individual at risk for sustaining a concussion.
Myth: All concussion treatments and recoveries are alike
Fact: No two concussions are identical. That’s why it's so important to take an individualized approach to concussion treatment.
Myth: You must be placed in a dark room to recover from a concussion.
Fact: Evidence-based, active treatments exist and generally patients do better when they are active sooner rather than later.
Signs and Symptoms of a Concussion
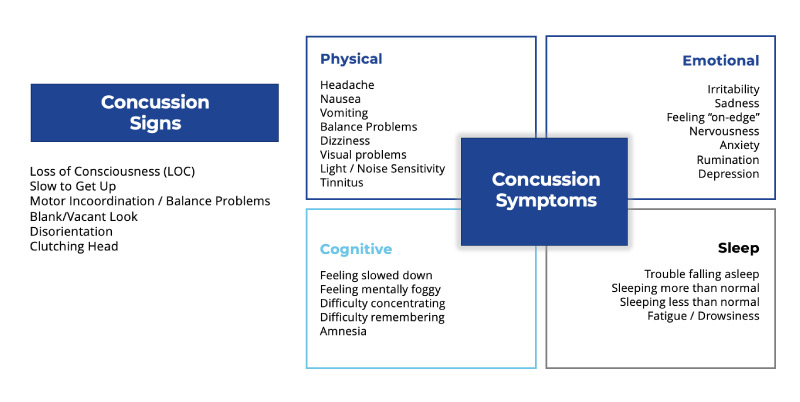
There are concussion signs and well as symptoms.
Common concussion signs:
- Loss of consciousness (LOC)
- Slow to get up
- Motor incoordination / balance problems
- Blank or vacant look
- Disorientation
- Clutching head
Common concussion symptoms are often grouped into 4 clusters: Physical, Emotional, Cognitive, and Sleep.
Physical symptoms:
- Headache
- Nausea
- Vomiting
- Balancing problems
- Dizziness
- Visual problems
- Light or noise sensitivity
- Tinnitus
Emotional symptoms:
- Irritability
- Sadness
- Feeling “on-edge”
- Nervousness
- Anxiety
- Rumination
- Depression
Cognitive symptoms:
- Feeling slowed down
- Feeling mentally foggy
- Difficulty concentrating
- Difficulty remembering
- Amnesia
Sleep symptoms:
- Trouble falling asleep
- Sleeping more than normal
- Sleeping less than normal
- Fatigue or drowsiness
When you see non-athletic patients presenting weeks or months after the injury, it’s important to consider the timeline in terms of when symptoms presented and how often they’re happening to ensure you’re seeing patterns consistent with what you’d typically see for a concussion versus another medical condition.
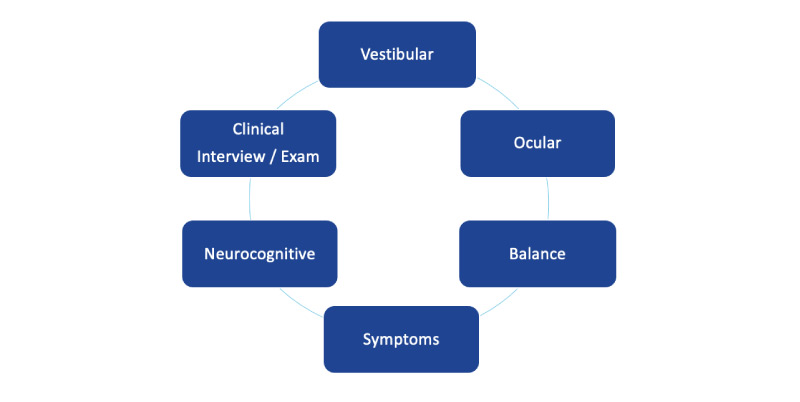
Multi-Faceted Concussion Assessment Approach
A multifaceted assessment approach is necessary to capture the heterogenic signs, symptoms, and impairments of a concussion because not every patient will present the same.
The multifaceted approach should include:
- Clinical interview and examination
- Neurocognitive testing
- Vestibular assessment
- Ocular assessment
- Balance assessment
- Detailed understanding of symptoms
It’s important to spend time with the patient and ask about other factors that could be influencing symptoms including pre-existing medical conditions and external stressors.
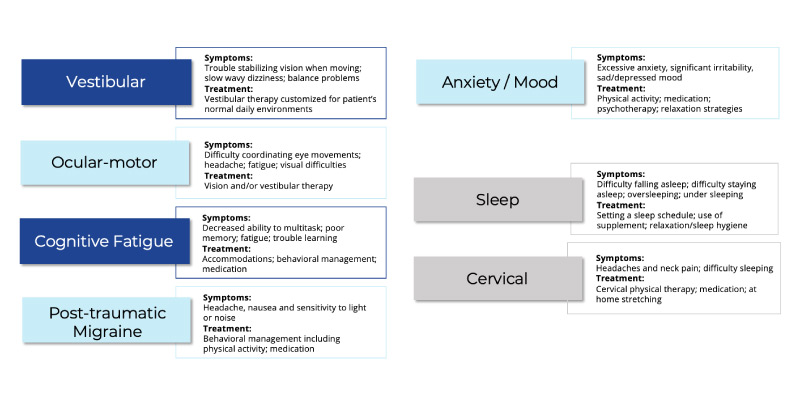
Concussion Clinical Profiles
There are 5 clinical profiles (also known as clinical trajectories):
- Vestibular
- Symptoms: trouble stabilizing vision when moving, dizziness, balance problems
- Treatment: Vestibular therapy
- Ocular Motor
- Symptoms: difficulty coordinating eye movements, frontal-based headaches, fatigue, visual difficulties
- Treatment: Vision and/or vestibular therapy
- Cognitive Fatigue
- Symptoms: (usually at the end of the day) overwhelming sense of fatigue, difficulty sleeping despite being so tired, decreased ability to multitask, trouble learning new information
- Treatment: workplace accommodations, school accommodations, getting patients into a routine regarding sleep, diet, hydration, physical activity, and stress management
- Post-Traumatic Migraine
- Symptoms: unilateral headache, nausea, noise / light sensitivity
- Treatment: getting patients on a regular schedule with emphasis on physical activity
- Anxiety and Mood
- Symptoms: excessive anxiety, significant irritability, feeling sad or depressed
- Treatment: increase physical activity, relaxation strategies, implementation of normal stress-relieving activities
In addition to the 5 clinical profiles, there are 2 clinical modifiers which can affect any of the other clinical profiles.
- Sleep
- Symptoms: difficulty falling asleep, difficulty staying asleep, oversleeping, undersleeping
- Treatment: setting a sleep schedule, relaxation techniques, sleep hygiene
- Cervical
- Symptoms:headache, neck pain, trouble sleeping because of neck pain
- Treatment: cervical physical therapy, home stretches
Your goal for the initial evaluation is to identify what clinical profile(s) are at play, if there are any clinical modifiers that may be influencing the profiles, and create an individualized treatment plan based on these findings.
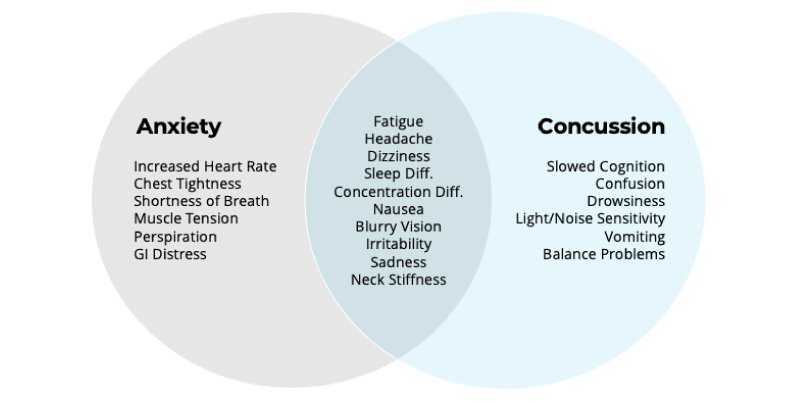
Concussions and Mental Health
American Psychological Association (APA) defines anxiety as “an emotion characterized by feelings of tension, worried thoughts, and physical changes like increased blood pressure.” Most patients will not recognize anxiety on their own, which is why you cannot be afraid to talk about it in order to understand how it may be influencing the clinical picture.
Anxiety can result in physical symptoms that can overlap with concussion symptoms including:
- Fatigue
- Headache
- Dizziness
- Sleep difficulties
- Concentration difficulties
- Nausea
- Blurry vision
- Irritability
- Sadness
- Neck stiffness
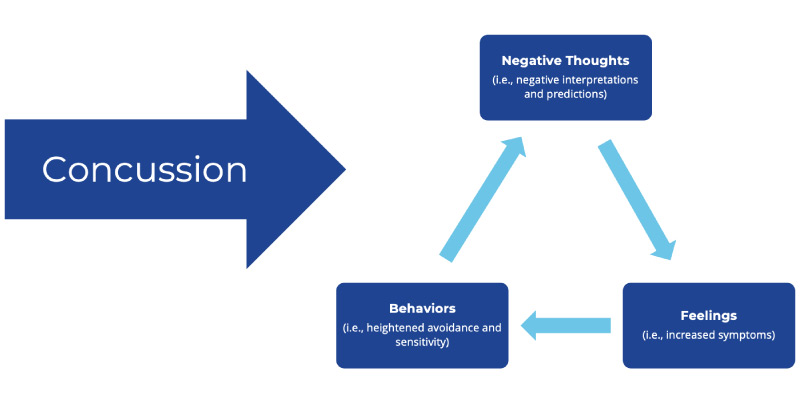
In addition to physical symptoms, anxiety can also influence how individuals process emotions. Following a concussion, patients may start to have negative thoughts or predictions which can lead to negative feelings and increase symptoms.
Many patients will try to avoid activities that bring them anxiety, which only maintains the anxiety over time.
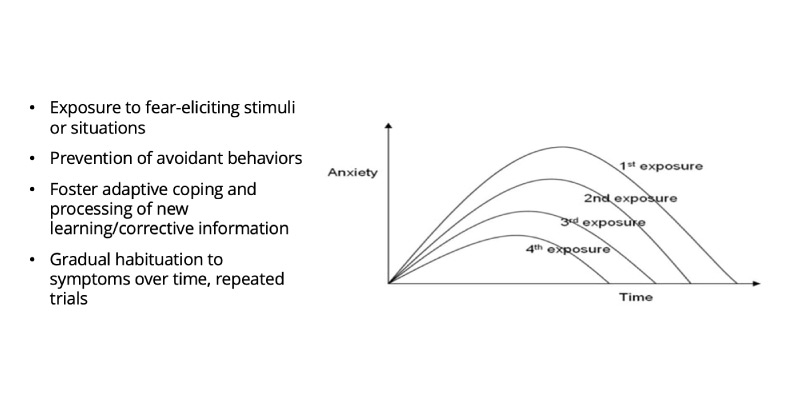
Instead, encourage patients to engage in active coping on a day-to-day basis with small exposures to the fear-eliciting stimuli. It’s helpful to ask family members to help identify some of the patient’s avoidant behaviors and encourage exposure. The more a patient is exposed, the less symptoms they should experience from those situations. Learn more about concussions and mental health in this comprehensive e-guide.
When to Return to Work After Concussion
Getting non-athletic patients back to work is just as important as getting student athletes back to sports and school in that it helps ease patients back into their normal routine. Once a patient’s symptoms become less severe (under 5/10 is the rule of thumb), they should be returning to work with appropriate accommodations.
Breaks should be used to manage symptoms. If patients are getting to a 5+ symptom severity, no matter what symptom that may be, they should take a break at that point. The break should consist of complete cognitive rest as much as possible (e.g. avoid using cellphone, chatting with coworkers, etc.) for about 10-15 minutes depending on the severity of symptoms.
Talk to patients about the benefit of returning to work even if they’re not 100%. Patients may be hesitant to go back to work, but easing back into their daily routine can actually help their recovery. If their employer will not allow them to return to work until they can return without accommodations, work with the patient to set up a home schedule that mirrors what they would be doing at work.
Talk to patients about their workplace environment. Understanding a patient’s work environment (e.g. are they in an individual office or an open work space?) will help you make appropriate modifications.
Progression is important. Depending on symptoms, you may suggest the patient start with part time before going back to full time work. If the patient’s job is very active, you may suggest they be placed on light-duty to begin (e.g. ICU nurse doing temperature checks).
Download the return to work quick reference guide.
For concussions that were the result of a workplace incident, you must be aware of the potential for legal involvement. Talking to patients about the benefits of interacting with a case manager can help them get access to treatments they may need.
When to Return to Driving After Concussion
After a concussion, patients may be experiencing cognitive deficits or physical symptoms that can impair their ability to drive. Cognitive tasks used in driving that may be affected by a concussion include reaction time, concentration, attention, visual perception, and memory. Physical symptoms that may impair driving include dizziness with head movements and decreased neck mobility. It’s also important to consider that patients whose concussion was from a motor vehicle accident (MVA) may have some level of anxiety or PTSD associated with getting behind the wheel again.
ImPACT provides objective measures of memory, reaction time, and processing speed which can be helpful in determining a patient’s readiness to return to driving. VOMS can also be helpful in determining the level of physical symptoms experienced with head movements.
Once you feel a patient is fit to return to driving, provide extra precautions that they should take such as:
- Practicing in a parking lot or on back roads
- Drive short distances
- Drive familiar routes
- Avoid driving at night
- Avoid additional distractions such as other passengers or music
Referral sources for non-athletic concussions may differ from those for sports related concussions. Some of the more common referral sources for non-athletic concussions include emergency rooms, urgent care facilities, primary care physicians, neurologists, physical therapists, chiropractors, and neuro-optometrists. Especially in non-athletic populations, patients may find you through word of mouth or by looking for a concussion specialist online.
It’s important to build your reputation as the go-to provider for concussion care services, so the community knows your facility is the place to go for concussion treatment.
Ensure you have the right team that can offer appropriate care for patients. Having a multidisciplinary team that’s trained in concussion care will allow patients to get the treatments they need under one roof which streamlines patient care. ( Download the multidisciplinary concussion care team quick reference guide)
Provide education sessions to referral sources. Offer concussion care training to urgent cares, primary cares, and other common referral sources in your community.
Provide concussion care resources to the community. Offer free ImPACT baseline testing and educational resources to individuals and organizations in the community.
Be able to see patients right away. Being able to see patients within days of their call is especially important when managing concussions. It’s also helpful to provide a hotline for patients to get their questions answered outside of business hours. This helps alleviate some of the fear and hysteria patients may be experiencing.
Be aware of your online presence. When patients and referral sources do an internet search, what will they find? Make sure your website is up-to-date with the latest concussion strategies and get your clinic listed in a reputable concussion care provider directory so patients can easily find you.
Want to learn more?
Take the CE-eligible, online webinar replay course, Concussion Care Beyond Athletics, and download 3 in-depth case studies.
Leave your email below and we’ll send you a promo code
to take it for free.
Beyond Athletics LP Email Course Promo Code